At least, we have the masks
A new study by researchers from the Max Planck Institute and Cornell University shows that FFP2 marks offer surprisingly effective protection against SARS-CoV-2. This is by all means great news, but I’m not sure that it will change anything in these times of aggressive anti-vaccinism and opposition to “the medical dictatorship”—as they call the entire set of prophylactic measures.
I first heard of the news last Saturday, on Dec. 4:
Important research from Max-Planck Institute: FFP2 masks, when worn tightly reduce risk of infection from being in close proximity for 20min to an infected person to 0,1%. Same setup with operation masks reduces to 4%. https://t.co/riYyhH09nL
— Ralitza (@inkscar) December 4, 2021
That’s a bit oversimplifying, though:
The article is somewhat incorrect, so here’s the original paper: https://t.co/Gd6OWvruMR
— Ralitza (@inkscar) December 4, 2021
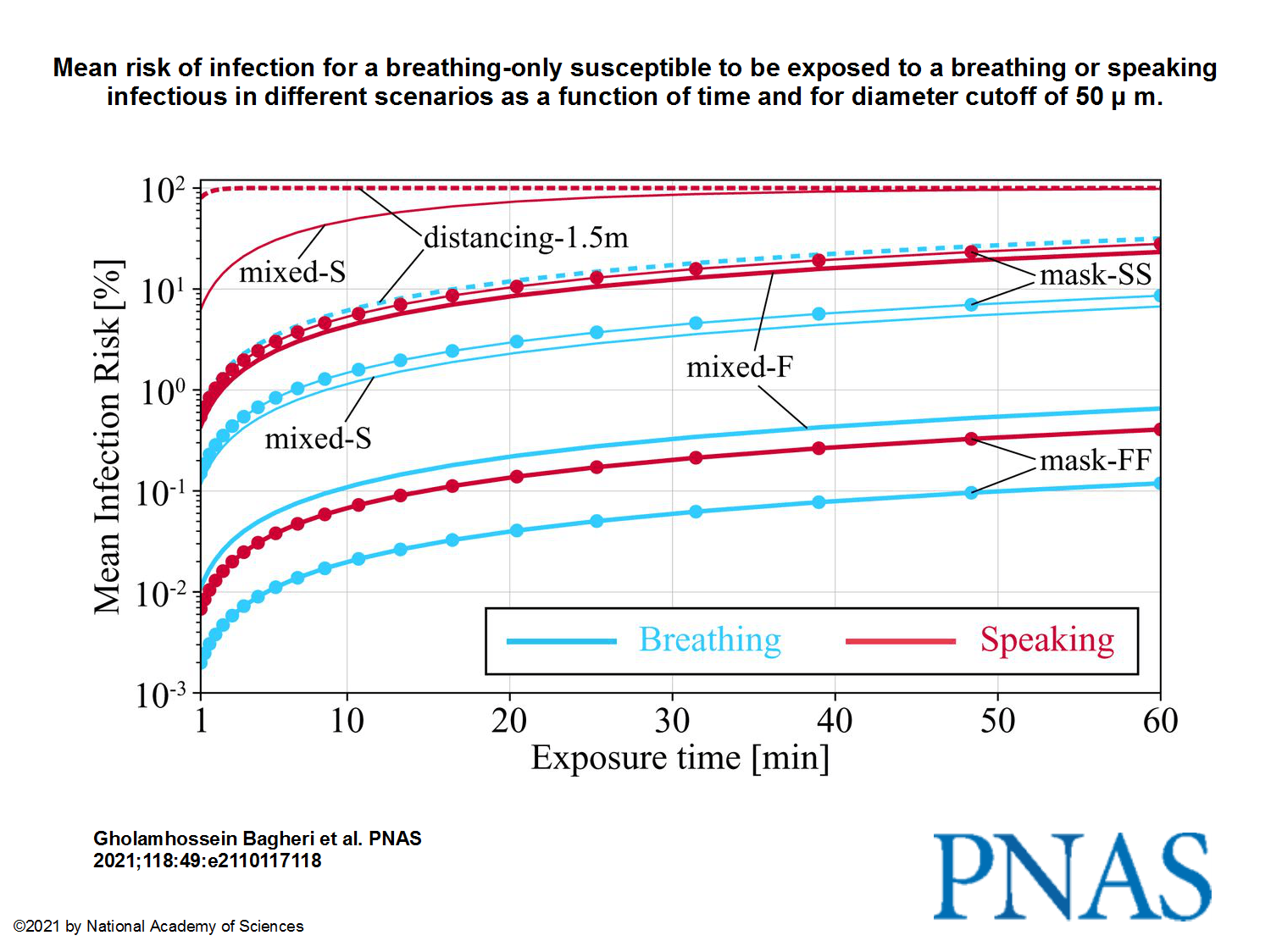
“When both wear a surgical mask, while the infectious is speaking, the very conservative upper bound remains below 30% after 1 h, but, when both wear a well-fitting FFP2 mask, it is 0.4%.”
Max Planck themselves:
The case for masking up: new study shows tight-fitting #FFP2 & vKN95 face masks drastically reduce the risk of #COVID19 infection – but even ill-fitting masks still significantly reduce the risk of infection https://t.co/vBb4JgBs76 @maxplanckpress pic.twitter.com/V2pkcfEc64
— Max Planck Society (@maxplanckpress) December 3, 2021
The press release by the Max Planck Institute for Dynamics and Self-Organization, Göttingen: How Well Masks Protect:
Three metres are not enough to ensure protection. Even at that distance, it takes less than five minutes for an unvaccinated person standing in the breath of a person with Covid-19 to become infected with almost 100 percent certainty. That’s the bad news. The good news is that if both are wearing well-fitting medical or, even better, FFP2 masks, the risk drops dramatically.
[…]
The Göttingen team was surprised at how great the risk of infection with the coronavirus is. “We would not have thought that at a distance of several metres it would take so little time for the infectious dose to be absorbed from the breath of a virus carrier,” says Eberhard Bodenschatz, Director at the Max Planck Institute for Dynamics and Self-Organisation. At this distance, the breathing air has already spread in a cone shape in the air; the infectious particles are correspondingly diluted. In addition, the particularly large and thus virus-rich particles fall to the ground after only a short distance through the air. “In our study we found that the risk of infection without wearing masks is enormously high after only a few minutes, even at a distance of three metres, if the infected persons have the high viral load of the delta variant of the Sars-CoV-2 virus,” says Eberhard Bodenschatz. And such encounters are unavoidable in schools, restaurants, clubs or even outdoors.
Well-fitting FFP2 masks reduce the risk at least into the per thousand range.
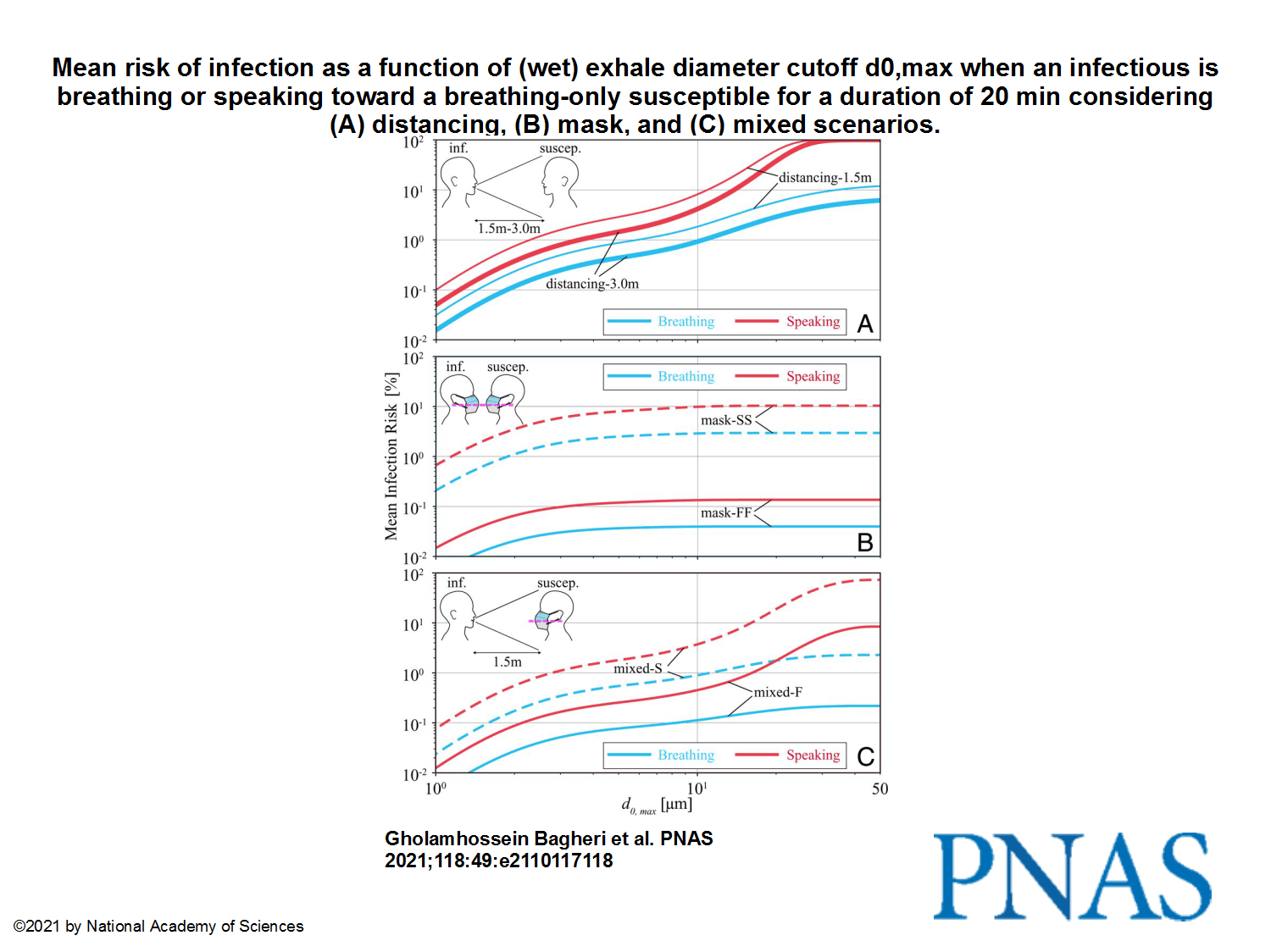
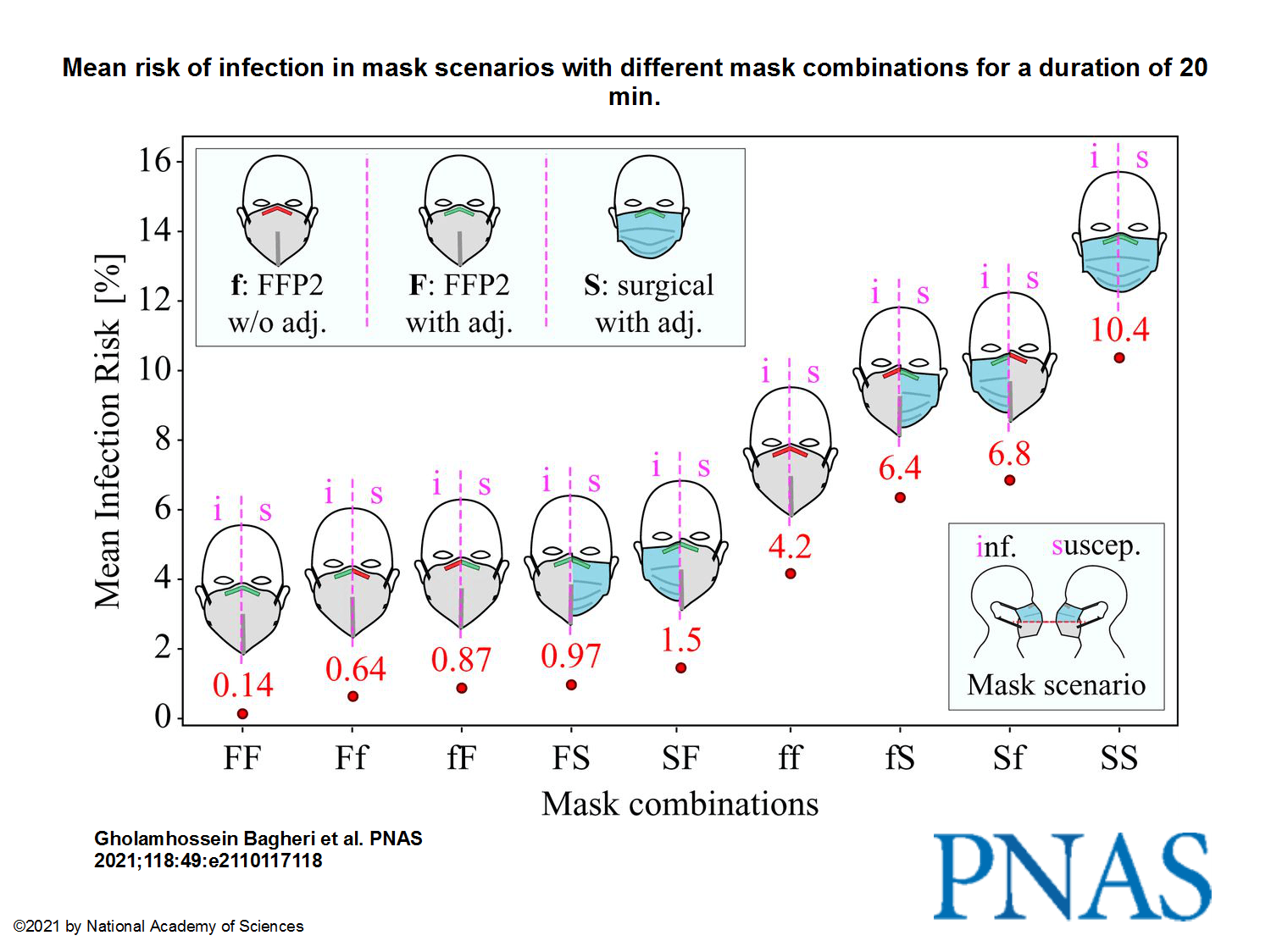
As high as the risk of infection is without mouth-nose protection, medical or FFP2 masks protect effectively. The Göttingen study confirms that FFP2 or KN95 masks are particularly effective in filtering infectious particles from the air breathed – especially if they are as tightly sealed as possible at the face. If both the infected and the non-infected person wear well-fitting FFP2 masks, the maximum risk of infection after 20 minutes is hardly more than one per thousand, even at the shortest distance. If their masks fit poorly, the probability of infection increases to about four percent. If both wear well-fitting medical masks, the virus is likely to be transmitted within 20 minutes with a maximum probability of ten percent. The study also confirms the intuitive assumption that for effective protection against infection, in particular the infected person should wear a mask that filters as well as possible and fits tightly to the face.
The infection probabilities determined by the Max Planck team indicate the upper limit of the risk in each case. “In daily life, the actual probability of infection is certainly 10 to 100 times smaller,” says Eberhard Bodenschatz. This is because the air that flows out of the mask at the edges is diluted, so you don’t get all the unfiltered breathing air. But we assumed this because we can’t measure for all situations how much breathing air from one mask wearer reaches another person, and because we wanted to calculate the risk as conservatively as possible,” Bodenschatz explains.
[…]
Although the detailed analysis by the Max Planck researchers in Göttingen shows that tight-fitting FFP2 masks provide 75 times better protection compared to well-fitting surgical masks and that the way a mask is worn makes a huge difference; even medical masks significantly reduce the risk of infection compared to a situation without any mouth-nose protection at all. “That’s why it’s so important for people to wear a mask during the pandemic,” says Gholamhossein Bagheri. And Eberhard Bodenschatz adds, “Our results show once again that mask-wearing in schools and also in general is a very good idea.”
To summarize:
- These are the maximum maximorum values of risk.
- 2 persons at 3 meters distance, no mask: the transmission is almost certain in 5 minutes!
- 2 persons, even at close distance, with FFP2/KN95 masks, correctly worn: the risk of infection after 20 minutes is less than 0.1%.
- Same as above, with incorrectly worn masks: the risk can go up to 4%.
- Using well-fitted surgical masks instead of FFP2/KN95: the risk can go up to 10%.
- More precisely, FFP2 masks are 75 times more effective than surgical masks if properly worn.
- In real life, you can be luckier by a factor of 10 to 100.
A pretty good article in German, by ZDF: Studie aus Göttingen – Wie gut schützen FFP2-Masken vor Corona?
As for the original study, An upper bound on one-to-one exposure to infectious human respiratory particles, let’s note that the researchers work for the following non-pharma institutions:
- Laboratory for Fluid Physics, Pattern Formation and Biocomplexity, Max Planck Institute for Dynamics and Self-Organization, Göttingen
- Institute for Dynamics of Complex Systems, University of Göttingen
- Laboratory of Atomic and Solid State Physics, Cornell University, Ithaca
- Sibley School of Mechanical and Aerospace Engineering, Cornell University, Ithaca
The abstract:
There is ample evidence that masking and social distancing are effective in reducing severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission. However, due to the complexity of airborne disease transmission, it is difficult to quantify their effectiveness, especially in the case of one-to-one exposure. Here, we introduce the concept of an upper bound for one-to-one exposure to infectious human respiratory particles and apply it to SARS-CoV-2. To calculate exposure and infection risk, we use a comprehensive database on respiratory particle size distribution; exhalation flow physics; leakage from face masks of various types and fits measured on human subjects; consideration of ambient particle shrinkage due to evaporation; and rehydration, inhalability, and deposition in the susceptible airways. We find, for a typical SARS-CoV-2 viral load and infectious dose, that social distancing alone, even at 3.0 m between two speaking individuals, leads to an upper bound of 90% for risk of infection after a few minutes. If only the susceptible wears a face mask with infectious speaking at a distance of 1.5 m, the upper bound drops very significantly; that is, with a surgical mask, the upper bound reaches 90% after 30 min, and, with an FFP2 mask, it remains at about 20% even after 1 h. When both wear a surgical mask, while the infectious is speaking, the very conservative upper bound remains below 30% after 1 h, but, when both wear a well-fitting FFP2 mask, it is 0.4%. We conclude that wearing appropriate masks in the community provides excellent protection for others and oneself, and makes social distancing less important.
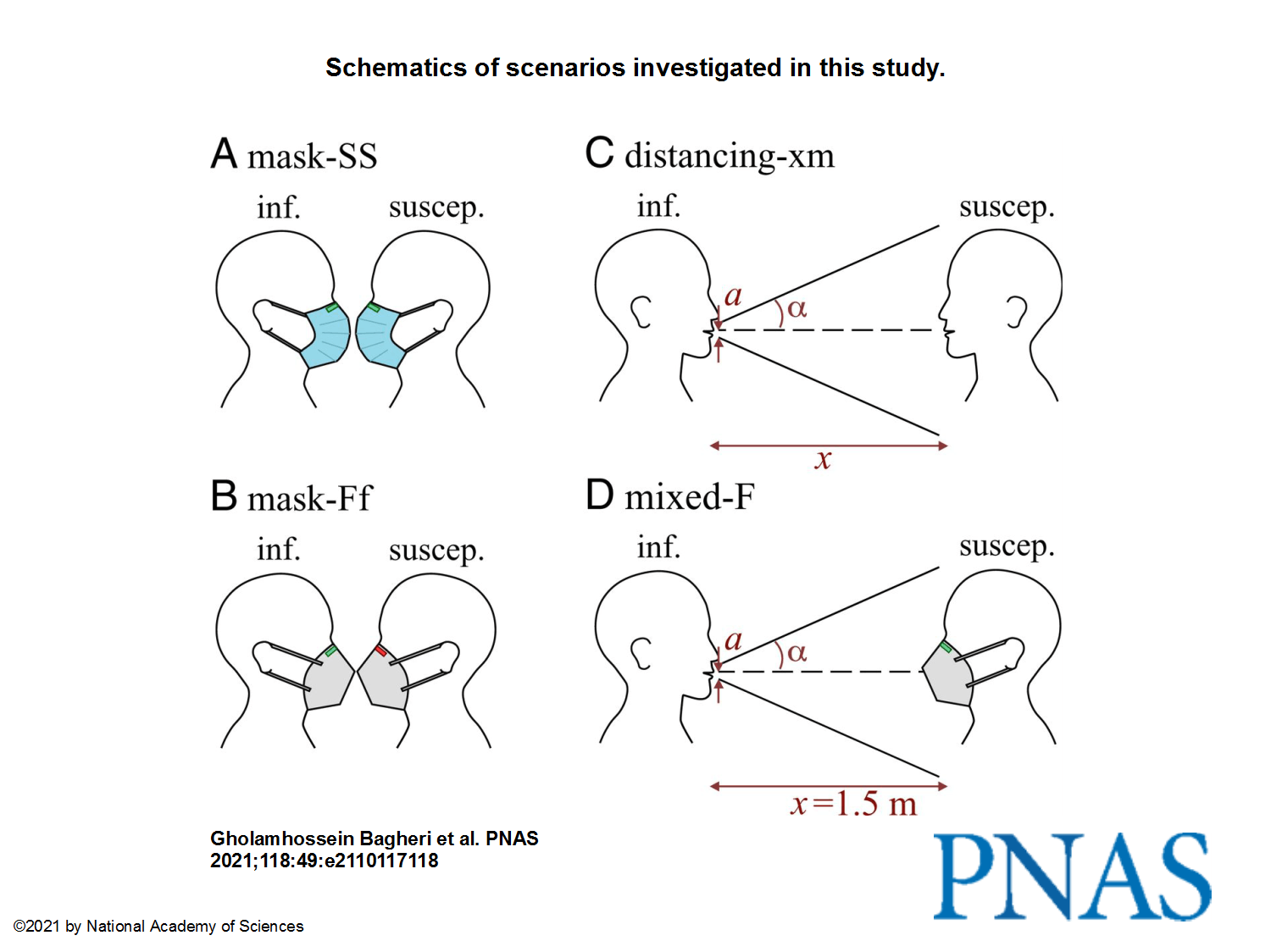
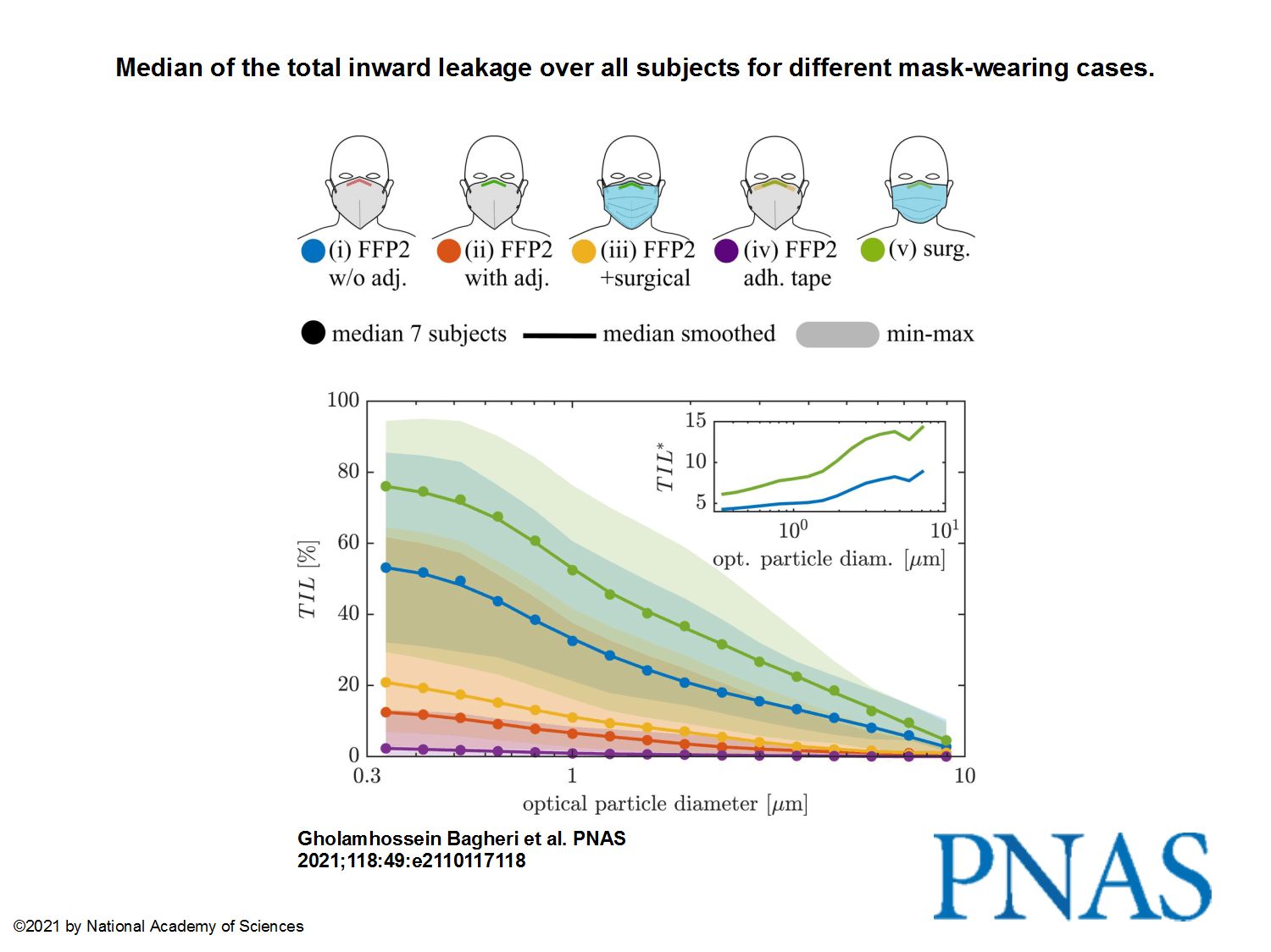
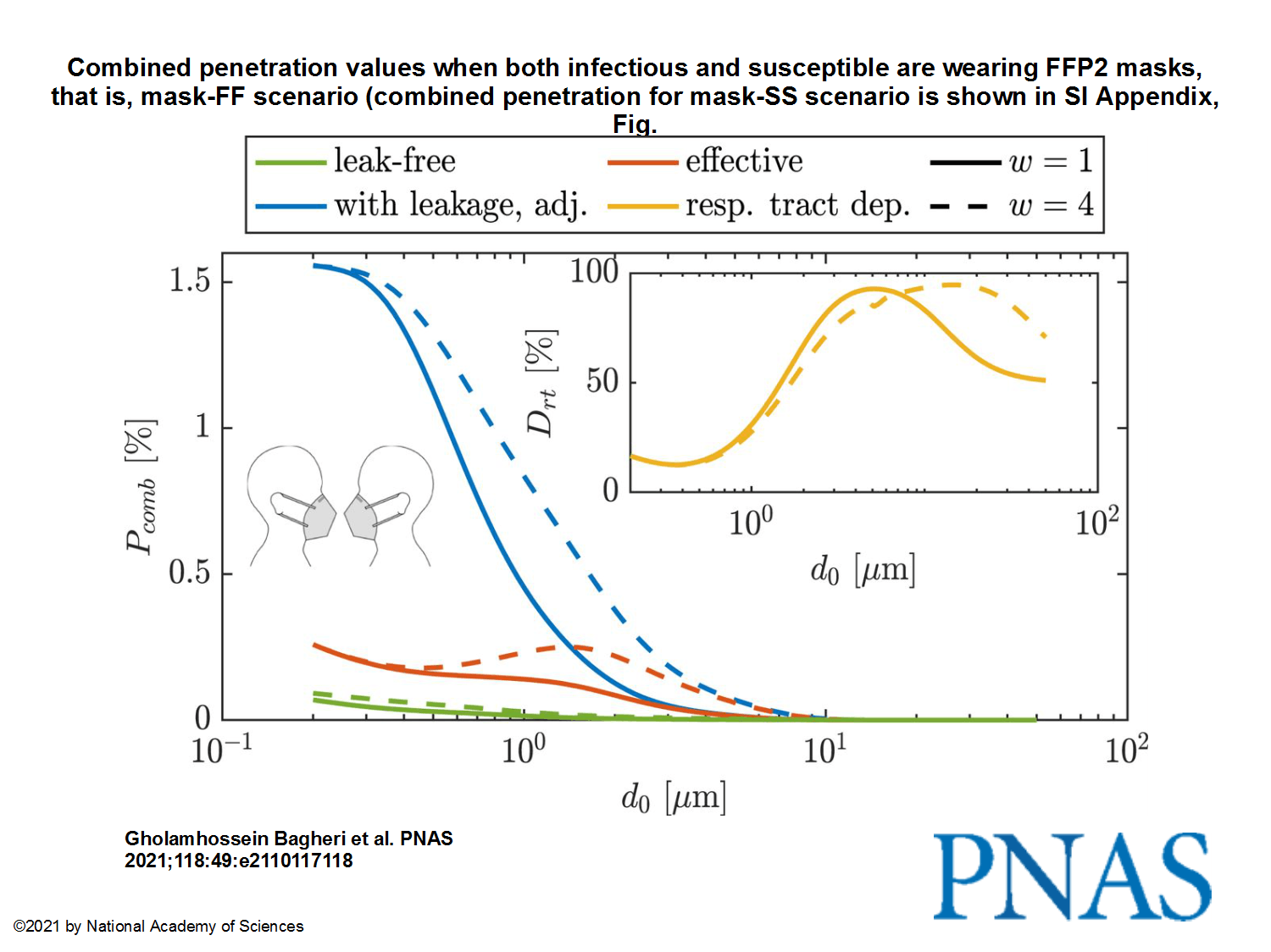
The images from the study, to pretend we have something to look at:
This being said, I’m not sure that anything really still matters nowadays, with all those reckless idiots fighting “for their freedom”! I surely hope they die of no matter what disease, as long as this happens because there’s no hospital to admit them or no doctor to take care of them.

Cred ca astia care intram pe aici suntem convinsi de purtarea mastii si vaccinare.